Pathophysiology of infectious diseases in diabetes mellitus
patients:
An overview
Tarawanti Verma1, Suman Ghosh 2, Saroj Singhmura 2*
B.S Anangpuria Institute of Pharmacy, Faridabad (Haryana)
Dr.B.C Roy College of Pharmacy and AHS, Durgapur (West Bengal)
*Correspondance
: saroj.singhmura@bcrcp.org
Abstract
Diabetes mellitus (DM) is a clinical syndrome
associated with deficiency of insulin secretion or action. It
occurs when the pancreas gland no longer produces the insulin
needed or it occurs
when it is not producing enough insulin and the insulin is not
working effectively. .
The diabetes mellitus patients are much more prone to infections
because of hyperglycemic condition .In hyperglycemic condition
there are several changes in our body
responsible for deleterious effects in immune defense mechanism. It
may result due to changes in leukocytes functions, complement
system and altered in microvascular responses
.
It has been found that diabetic patients are susceptible to
different infectious diseases, such as
Malignant external otitis. Rhino cerebral mucormycotic, Gangrenous
cholecystitis
, Respiratory infections. Urinary tract infections.
Gastrointestinal and liver infections. This review enlightens the
pathophysiology and the infectious diseases which being responsible
for morbidity of diabetic patients.
Keywords
: hyperglycemic, polymorphoneutrophils (PMN),
complement system
INTRODUCTION
Diabetes mellitus is a disorder occurs due to metabolic problems and is
most frequent globally. The main indication of diabetes mellitus is a
hyperglycemia in blood which is due to inappropriate pancreatic insulin
secretion or low insulin-directed fostering of glucose by target cells.
Diabetes mellitus can be assorted into several types, but the two major
types are type 1 and type 2.Type 1 DM or insulin-dependent diabetes
mellitus (IDDM) in which body fails to produce insulin, and presently
requires the person to inject insulin or wear an insulin pump. Type 2
DM or non-insulin-dependent diabetes mellitus (NIDDM), results from
insulin resistance, a condition in which cells fail to use insulin
properly, with or without an absolute insulin deficiency.
India is amongst the top most countries followed by China and USA where
Diabetes still plagues the society with 32, 26 and 18 million cases
respectively[1]. In India, data state that diabetes going to affects
every 5th individual by 2025(40 million diabetes is expected
to be 70 million by 2025) [2]. World scenario as per WHO report, says
the prevalence of diabetes cases were increasing, where 1.5 million
deaths were estimated in the year 2012 directly from diabetes and it is
predicted that it will be the 7th leading cause of death in
2030[3]. Thus knowing the pathophysiology and its risk factors which
increases the morbidity need to be elaborately study.
Pathophysiology of diabetes
Type 1 diabetes mellitus
Several factors that causes diabetes such as increased carbohydrate
uptake or hepatic glucose production has been summarized in Fig. 1.
Characterized by autoimmune destruction of insulin producing cells in
the pancreas. The body’s own immune system ,which normally fights
harmful viruses and bacteria ,mistakenly destroys insulin producing
cells such as islet or islets of Langerhans in the pancreas. When a
significant number of cells are destroyed, produce little or no
insulin. Causes of the presence of certain genes indicates an increased
risk of developing type 1 diabetes. Exposure to viruses and other
environmental factors may also leads to type 1 diabetes. When there is
a deficiency in insulin leads to uncontrolled lipolysis and elevated
levels of free fatty acids in the plasma, which suppresses glucose
metabolism in peripheral tissues such as skeletal muscle. This impairs
glucose utilization and insulin deficiency also decreases the
expression of several genes necessary for target tissues to respond
normally to insulin such as glucokinase in liver.
Type 2 diabetes mellitus
In this dysfunction of the pancreatic β-cell occur, inadequate amounts
of insulin and impaired insulin action through insulin resistance.
Insulin resistance refers to when cells of the body such as liver, fat
cells and muscle fail to respond to insulin. The plasma insulin
concentration is insufficient to maintain normal glucose homeostasis.
Insulin resistance and hyperinsulinemia eventually lead to impaired
glucose tolerance. Inherited as an autosomal dominant trait, may result
from mutations in glucokinase gene on chromosome. Although genetics and
environmental factors such as excess weight and inactivity seem to be
contributing factors. Type 2 diabetes can be hereditary.
Fig. 1:
Factors cause increase blood glucose level.
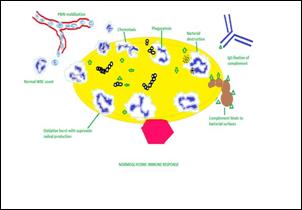
Immune responses to hyperglycemic Condition
In search for the answer of why hyperglycemic environment in diabetic
patients is more susceptible to infection. From earlier reported study,
it was found that this situation is responsible for deleterious effects
in immune defense mechanism. It may result due to changes in
(a)leukocytes functions, (b)complement system and altered in
microvascular responses (Fig. 2A, 2B)
Effects in leukocytes functions
: Hyperglycemic environment in diabetic patient may affects the
leukocytes functions in many ways like decreasing chemotaxis,
phagocytosis, adherence and bactericidal activity.
Chemotaxis is considered as an important mechanism for mobilizing
immune cells and phagocytic as an immune reaction at sites of
infection, tissue injury [4]. From earlier study it has been observed
that, chemotaxis is inhibited by hyperglycemic condition and this is
reversed in case when treated in control insulin [5-7]. Reports shows
in an animal models, hyperglycemia caused impairment of phagocytosis in
both monocytes and granulocytes and the immune dysfunction was
partially reversed by insulin [8]. In another reports
also shows that, in hyperglycemic condition glucose 6-phospate
dehydrogenase (G6PD) is inhibited reflects its antimicrobial action,
also increases apoptosis of polymorphonuclear leukocytes and reducing
polymorphonuclear leukocyte transmigration through the endothelium [9].
Many reports show that in both diabetics and in hyperglycemic
environment, the bactericidal activity of neutrophils is decreased in
environments. This may vary, however, with the organisms being
investigated [10, 11]. Respiratory burst (sometimes
called oxidative burst) is the rapid release of
reactive oxygen species
, plays an important role in the immune system
. Report shows that high glucose concentrations in vitro cause
inhibition of PMN respiratory oxidative burst. Result the decreased of
intracellular pathogen lysis that occurs during hyperglycemia.
Phagocytosis is also impaired by decreased oxidative burst generation
in monocytes [8, 12].
Effects in complement system:
It is a part of an immune system that is responsible for the enhancing
the ability of phagocytic cells and antibodies to clear microbes. The
stimulation of phagocytes, as a result of complement activation cascade
cause clear of foreign and damaged material and inflammation to attract
additional phagocytes, and
activation
of the cell-killing
membrane attack complex
. The complement system consist of more than 30 proteins and protein
fragments, including
serum proteins
, and
cell membrane receptors
. The
classical complement pathway
, the
alternative complement pathway
, and the
lectin pathway
are the biochemical pathway that activate the complement system. The
intricate
complement system
involved, human Complement component 4 (C4),which is a protein,
originating from the
human leukocyte antigen
(HLA) system. It works for several critical functions in immunity,
tolerance, and autoimmunity with the other numerous components.
Furthermore, it is a crucial factor in connecting the recognition
pathways of the overall system instigated by antibody-antigen (Ab-Ag)
complexes to the other effector proteins of the innate immune response.
For example, the severity of a dysfunctional complement system can lead
to fatal diseases and infections.
From earlier reports it has shown deficiency of C4 component in
diabetes [13]. The deficiency may be due to polymorphonuclear
dysfunctions and reduced cytokine [14,15]. In another study, it was
found that hyperglycemic conditions inhibit C3-mediated complement
effects in bacterial infection and this is due to glycosylation of the
C3 element, The conditions of elevated glucose cause C3 to undergo
structural changes affecting the immune response in hyperglycemic
environment [16,17].
Altered Microvascular responses:
The effectiveness of an immune response depends not only on the proper
activation, regulation, and function of immune cells, their
distribution in diverse tissue microenvironments is also very
important, where they encounter a number of stimuli and other cell
types. Endothelial cells are responsible for these activities, which
form specialized microcirculatory networks used by immune cells under
both physiological and pathological circumstances. Both conditions are
proinflammatory, leads to increased levels of TNF-alpha, IL-6, and
IL-8. While inflammatory responses are important in eradication of
infectious agents, the
resulting edema can lead to hypoxia as well as microvascular and
macrovascular dysfunction. [18,19,20]. Reports also indicates that nitric
oxide production is also hampered in hyperglycemic condition and as
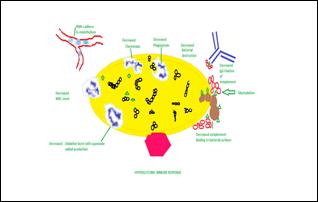 Fig. 2
Fig. 2
: Showing changes in immune responses due to hyperglycemic environment,
A: Normoglycemic Immune Response B: Hyperglycemic Immune Response
(picture taken and modified from Ashley M. Shilling et al., 2008)
 a result it cause failure of vasodilation which may result in
preventing phagocytes to reach the infection site/ target [21].
a result it cause failure of vasodilation which may result in
preventing phagocytes to reach the infection site/ target [21].
INFECTIONS IN DIABETES
In diabetes mellitus, there are some infections frequently arising and
this has increased the risk of altered immune response due to
hyperglycemia. There are number of rare but potentially fatal
infections occur primarily or even almost exclusively in patients with
diabetes. These include emphysematous urinary tract infections, Rhino cerebral mucormycotic, emphysematous
cholecystitis, necrotizing fasciitis and malignant otitis externa
(Table 1).
Malignant external otitis
It is an aggressive and potentially life-threatening infection of the
soft tissues of the external ear and surrounding structures. Causative
organism is Pseudomonas aeruginosa, begins with external
otitis that progresses into an osteomyelitis of the temporal bone.
Spread the diseases outside the external auditory through Santorini and
osseocartilaginous junction. It occurs more in old diabetic and
immune-compromised patients (Fig 3). Facial paralysis (Fig. 4) is
occurred in 50% cases. The best diagnostic method is the magnetic
resonance imaging. [22-23] (http://www.drmkotb.com)
Rhino cerebral mucormycotic
It is a rare opportunistic and invasive infection. This infection
occurs in 50% of the cases approx. Individual with DM due to
greater availability of glucose causes

Fig. 3
Malignant otitis externa

Fig. 4
Paralysis especially facial nerve
Mucormycotic. Caused by fungi of the class Zygomycetes. Classical triad
are paranasal sinusitis, ophthalmoplegia with blindness, unilateral
proptosis with cellulitis Black necrotic eschar in the nasal cornets
characteristic sign. Facial or eye pain and necrotic wound of the
palate of the nasal mucosa may occur. commonly affects individuals with
diabetes and those in immunocompromised states [23-24]
|
Table 1. Infectious Disease in Diabetic Patients
Gastrointestinal and liver infections
H. Pylori
infection
Oral and esophageal candidiasis
Emphysematous cholecystitis
Hepatitis c
Hepatitis b
Enteroviruses
Respiratory infections
Streptococcus pneumoniae
Influenza
H1n1
Tuberculosis
Urinary tract infections
Acute Pyelonephritis
Asymptomatic bacteriuria
Fungal cystitis
Renal Emphysema
Emphysematous cystitis
Perinephric abscess
Head and neck infections
Invasive external otitis
Rhinocerebral mucormycosis
Skin and soft tissue infectios
Pyomyositis
Malignant External Otitis
Foot infection
Necrotizing fasciitis
Fournier's gangrene
Bacterial infections:
- Styes
- Boils folliculitis
- Carbuncles
- Infections around the nails
Fungal infections
- Ringworm
- Jock itch
- Vaginal yeast infection
- Athlete’s foot
Other infections
Human immunodeficiency virus
Oral Infections
Surgical Infections
|
Emphysematous urinary tract infections
Emphysematous cystitis and pyelonephritis consider to be rare but most
dangerous complications of common urinary tract infection. Those who
has poorly controlled diabetes suffered from this rare infection,
raising chances more than 95% of patients with an emphysematous urinary
tract infection. The causative organism is E. Coli and constitute in
70% of cases [25] Suffering patients might have, fever to persists
despite adequate antimicrobial therapy. With the help of CT scan gas
formation in the pyelum or bladder wall can be diagnosed. Hyperglycemia
result Gas formation and impaired blood supply, in combination in the
presence of gas forming bacteria, facilitating anaerobic metabolism.
For emphysematous cystitis Antibiotic treatment alone is mostly enough
but Emphysematous pyelonephritis should be treated with adequate
antibiotic treatment in combination with either percutaneous drainage
or nephrectomy. Mortality is between 7 and 13%, despite adequate and
immediate treatment.
Emphysematous cholecystitis
It is a rare infection affecting men. About 40% diabetic patients
experienced emphysematous cholecystitis. The diagnosis is usually made
with (ultrasound, x-ray or CT scan). Causative organism areClostridium species, E coli, and Klebsiella species. In case of emphysematous cholecystitis,
rapid cholecystectomy should be performed. In case of an unacceptably
high surgical risk, percutaneous drainage can be considered. Mortality
of emphysematous cholecystitis is estimated to be around 15%, compared
to 4% of patients with non-emphysematous cholecystitis.
Necrotising fasciitis
It is another rare soft tissue infection. it is fatal in 20-40%
diabetic patient [25]. About 70% of patients with necrotising fasciitis
has diabetes mellitus. Necrotising fasciitis of the genital, perineum
and perianal region is also named ‘Fournier’s gangrene.’ The clinical
presentation is erythematous skin discoloration and low grade fever.
Pain may be disproportionately severe for the physical findings. When
crepitus and hematologic bullae appear a few days later, the disease is
likely to be fatal. Rapid intervention with antimicrobial treatment in
combination with extensive surgical intervention is essential.
Causative organism is Staphylococcus aureus, beta haemolytic
streptococcus bacteria, and vibrio bacteria are most common.
CONCLUSION
Diabetic patients are compromise of infectious disease due to
hyperglycemic environment, which suppress the immune response resulting
in number of fatal infectious diseases which commonly occur in diabetic
patients like malignant external otitis, Rhinocerebral mucormycosis,
and gangrenous cholecystitis, this increases the chances of morbidity
and mortality. Thus, diabetic patients’ complication is to be identify
promptly to control the hyperglycemic environment and possible
treatment can be provided. But still the extent diabetic patients
increase the risk of infections is still controversial due to lack of
controlled clinical studies. Thus, more clarification is required to
understand the immunopathogenic mechanism related to diabetes patients.
REFERENCES
- “Collaborative framework for care and control of tuberculosis and
diabetes”. WHO Global Report; 2011:39
- “Definition and Diagnosis of diabetes mellitus and intermediate
hyperglycaemia”. Report of a WHO/IDF consultation; 2006:50
- A.S. Prank, G. Halade, S. Kumar, R. Mogre, K. Apte, A.D.B Vaidya,
B. Patwardhan, Cassia auriculate: aspects of safety
pharmacology and drug interaction, Evid. Based. Complement.
Alternat. Med. 2011 (2011) 915240
- Function and Regulation of Tor Complexes from Yeasts to Mammals
Part B, Ed: MN Hall, F Tamanai, Part B, Academic Press, 2010
- A. Mowat, J. Baum, Chemotaxis of polymorphonuclear leukocytes from
patients with diabetes mellitus, The New Eng J. Med. 284 (1971)
621–627.
- J.D. Bagdade, R.K. Root, R.J. Bulger, Impaired leukocyte function
in patients with poorly controlled diabetes, Diabetes. 23 (1974)
9–15.
- M. Delamaire, D. Maugendre, M. Moreno, M.C. LeGoff, H. Alannic, B.
Genetet. Impaired leucocyte functions in diabetic patients,
Diabetic Med. 14 (1997) 29–34.
- B. Ellger, Y. Debaveye, I. Vanhorebeek, L. Langouche, A. Giulietti,
E. Van Etten, P. Herijgers, C. Mathieu, G. Van den Berghe. Survival
benefits of intensive insulin therapy in critical illness: impact
of maintaining normoglycemia versus glycemia-independent actions of
insulin, Diabetes 55 (2006) 1096–1105
- A.Y. Peleg, T. Weerarathna, J.S. McCarthy, T.M. Davis. Common
infections in diabetes: Pathogenesis, management and relationship
to glycaemic control, Diabetes Metab. Res. Rev. 23 (2007) 3-13.
- D. Balasoiu, K.C. van Kessel, H.J. van Kats-Renaud, T.J. Collet,
A.I. Hoepelman. Granulocyte function in women with diabetes and
asymptomatic bacteriuria. Diabetes Care 20 (1997) 392–395.
- J.S. Tan, J.L. Anderson, C. Watanakunakorn, J.P. Phair. Neutrophil
dysfunction in diabetes mellitus. The J. Lab. Clinical. Med. 85
(1975) 26–33.
- J.D. Bagdade, E. Walters, Impaired granulocyte adherence in mildly
diabetic patients: effects of tolazamide treatment, Diabetes 29
(1980) 309–311.
- M. Stoeckle, C. Kaech, A. Trampuz, W. Zimmerli, The role of
diabetes mellitus in patients with bloodstream infections. Swiss
Med Wkly 138 (2008) 512-519.
- S.E. Geerlings, A.I. Hoepelman, Immune dysfunction in patients with
diabetes mellitus (DM). FEMS Immunol. Med. Microbiol. 26 (1999)
256-265
- M. Stoeckle, C. Kaech, A. Trampuz, W. Zimmerli, The role of
diabetes mellitus in patients with bloodstream infections, Swiss.
Med. Wkly. 138 (2008) 512-9.
- P.S. Hair, C.G. Echague, R.D. Rohn, N.K. Krishna, Hyperglycemic
conditions inhibit C3-mediated immunologic control of Staphylococcus aureus, J Transl Med. 10 (2012) 35.
- M.K. Hostetter, Handicaps to host defense. Effects of hyperglycemia
on C3 and Candida albicans. Diabetes 39 (1990): 271–275.
- K. Esposito, F. Nappo, R. Marfella G. Giugliano, F. Giugliano, M.
Ciotola, L. Quagliaro, A. Ceriello, D. Giugliano. Inflammatory
cytokine concentrations are acutely increased byhyperglycemia in
humans: role of oxidative stress. Circulation 106 (2002) 2067–2072.
- D. Zozulinska, A. Majchrzak, M. Sobieska, K. Wiktorowiz, B.
Wierusz-Wysocka, Serum interleukin-8 level is increased in diabetic
patients. Diabetologia 1999; 42: 117–118.
- A.D. Mooradian, R.L. Reed, Meredith KE, P. Scuderi, Serum levels of
tumor necrosis factor and IL-1 alpha and IL-1 beta in diabetic
patients. Diabetes Care 14 (1991) 63–65.
- S.B. Williams, A.B. Goldfine, Timimi FK, H.H. Ting, M.A. Roddy,
D.C. Simonson, M.A. Creager, Acute hyperglycemia attenuates
endothelium-dependent vasodilation in humans in vivo. Circulation
97 (1998) 1695–1701.
- S.E. Geerlings, A.I. Hoepelman, Immune dysfunction in patients with
diabetes mellitus (DM) FEMS immunol. Med. Microbiol. 26 (1999)
256-265.
- L.M. Muller, K.J. Gorter, E. Hak, W.L. Goudzwaard, F.G. Schellevis,
A.I. Hoepelman,et al. Increased risk of common infections in
patients with type 1 and type 2 diabetes mellitus. Cin Infect Dis.
2005;41:
- J. Casqueiro, J. Casqueiro, C. Alves, Ind. J. Endcrinology Metab.
16 (2012) S27-S36.
- S.S. Ubee, L. McGlynn, M. Fordham, Emphysematous pyelonephritis,
BJU Int. 107 (2011):1474–8.